

Advanced Wound Dressings: What Sets Them Apart?
Introduction
At R&L Medical, we believe wound care is entering a new era. Traditional bandages and gauze once served as the primary option for wound management, but they often fell short in addressing modern clinical needs. Patients require solutions that not only protect against contaminants but also create an environment where the body can heal efficiently and comfortably. This is where advanced wound dressings come into play. These innovative products are designed to support faster recovery, reduce infection risks, minimize dressing changes, and enhance patient comfort.
This article will explore the fundamentals of wound dressings, explain what makes advanced dressings different, and highlight specific applications in surgical recovery, diabetic ulcer management, and orthopedic procedures. We will also introduce R&L Medical’s Visual Waterproof Dressing, a next-generation solution that combines visibility, waterproofing, high absorbency, and breathability to set a new standard in wound care.
Wound Dressing
A wound dressing is not simply a cover for an injury; it is an essential component of the healing process. The core functions of any wound dressing include:
-
Protection: shielding the wound from bacteria, dirt, and external contaminants.
-
Moisture balance: ensuring the wound environment supports cell regeneration.
-
Exudate management: absorbing wound fluids to prevent maceration of surrounding skin.
-
Comfort: reducing pain, friction, and irritation.
Traditional dressings such as gauze pads or adhesive bandages provide a basic barrier but often require frequent changes, may dry out wounds, and can stick to healing tissue, causing trauma during removal. This is why the transition to advanced wound dressings marks such a significant improvement in wound care.
Advanced Wound Dressings
Advanced wound dressings are engineered to go beyond simple coverage. They are constructed using innovative materials such as hydrocolloids, foams, alginates, transparent films, and antimicrobial compounds. Each type is tailored to specific wound conditions and offers benefits like prolonged wear time, enhanced comfort, and improved clinical outcomes.
Key characteristics that set advanced wound dressings apart include:
-
Moist wound healing: maintaining the right balance of hydration for faster tissue repair.
-
Reduced infection risk: providing a secure barrier against bacteria and viruses.
-
Longer wear time: minimizing the frequency of dressing changes, which reduces disruption to the wound.
-
Patient-centered design: flexibility, breathability, and low allergenic potential for improved quality of life.
At R&L Medical, our mission is to lead in this new generation of wound care, offering products that deliver these benefits in real clinical practice.
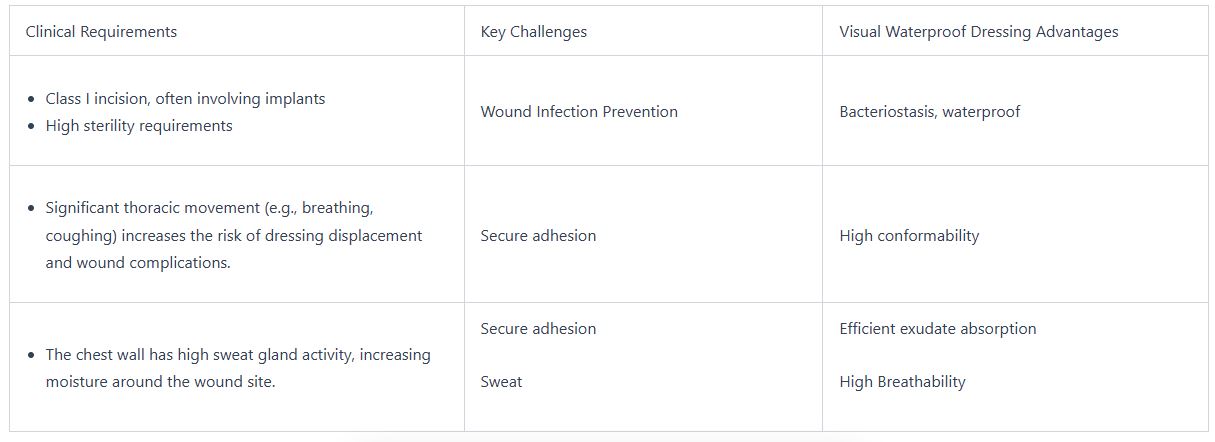
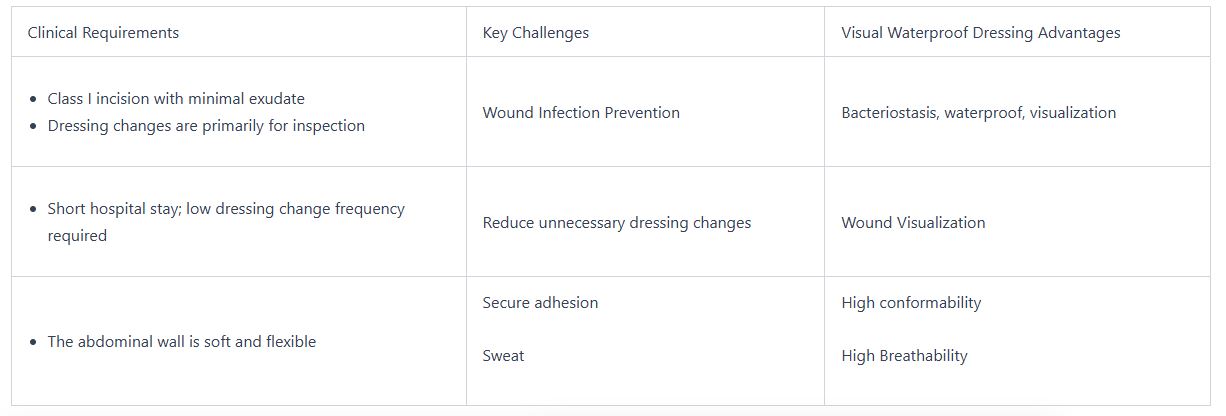
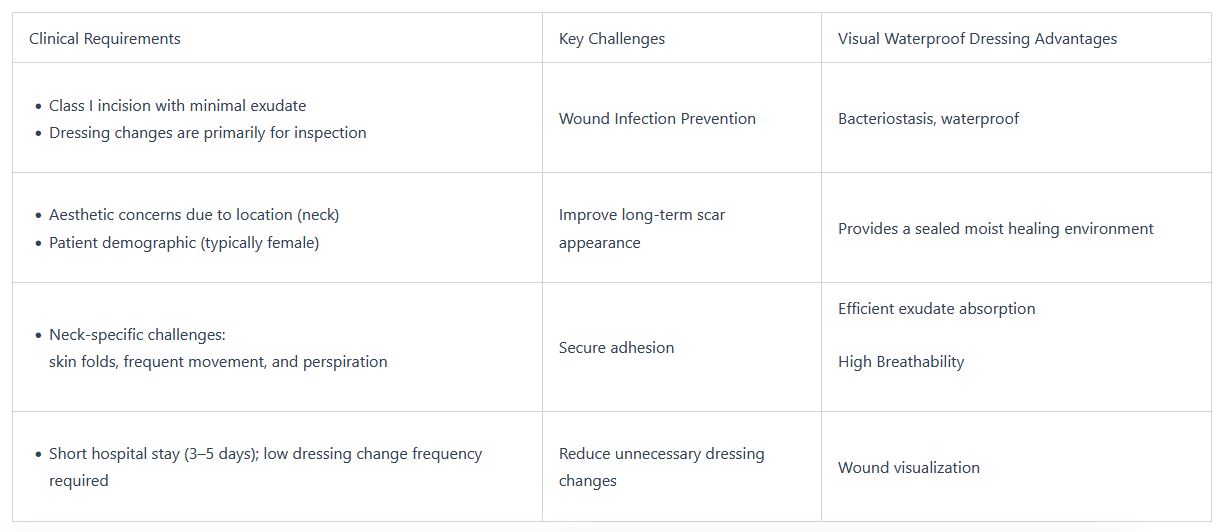
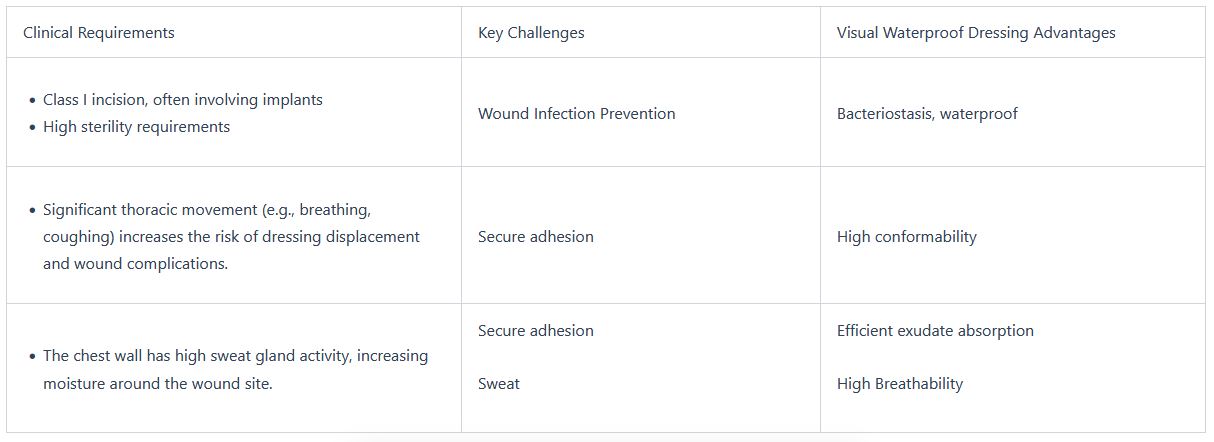
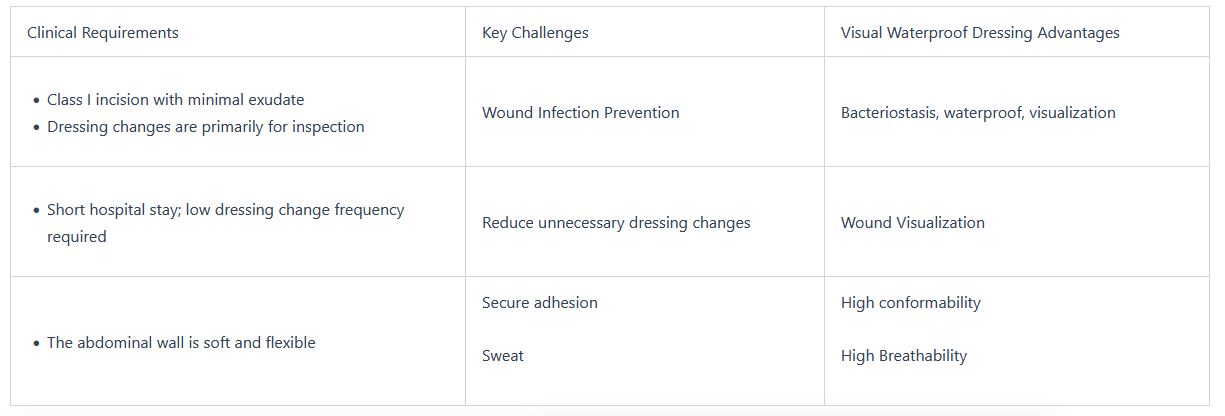
Post Surgical Wound Dressing
Surgical wounds present unique challenges. They must remain protected from bacteria while the incision heals, but they also need to allow physicians to observe the site for signs of infection or dehiscence (wound reopening). Post-surgical dressings should:
-
Provide waterproof and bacteria-resistant protection.
-
Offer gentle adhesion to avoid damaging delicate skin during removal.
-
Stay securely in place over moving body parts.
-
Reduce the frequency of dressing changes to minimize infection risk and improve comfort.
Our dressings play an important role in postoperative recovery by protecting the incision and supporting faster, cleaner healing. They are especially suitable for surgical sites with low to moderate exudate, helping maintain a moist healing environment while preventing contamination. At R&L Medical, we design dressings that balance secure adhesion with comfort, ensuring patients can recover confidently at home.
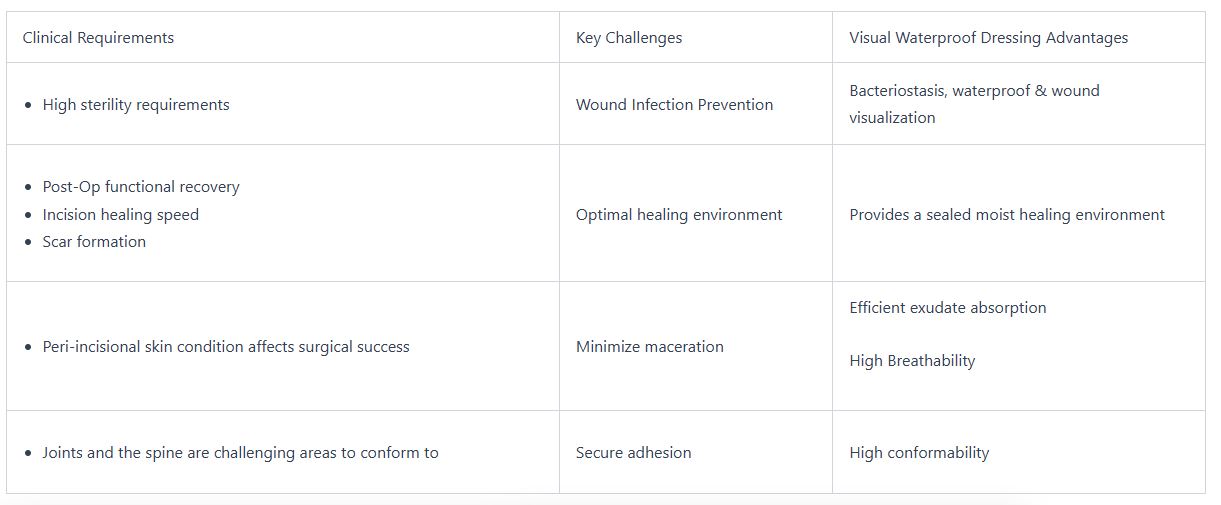
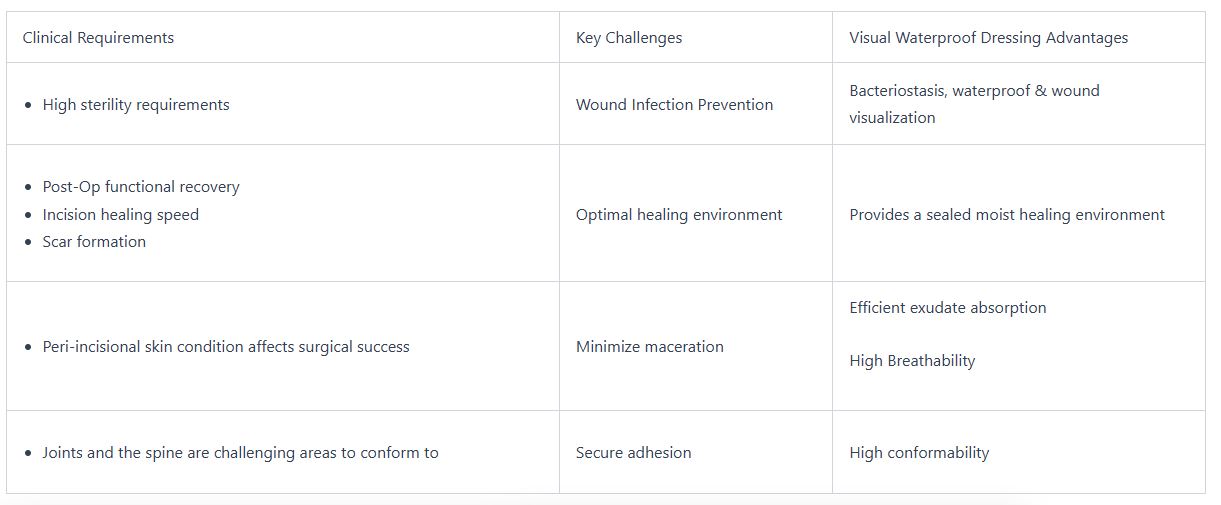
Advantages of visual waterproof dressings for this type of disease
-
Flexible: conforming to knee movement without losing adhesion.
-
Absorbent: capable of managing moderate exudate during the early recovery period.
-
Waterproof: enabling patients to maintain hygiene and shower without compromising protection.
-
Durable: remaining intact despite bending and stretching.
Orthopedic Applications:Joints
When and Why Change Dressing on Wound
Changing a wound dressing is more than just a scheduled task; it is also an opportunity to assess the healing process and identify potential complications early. Each dressing change gives clinicians and patients the chance to evaluate how well the wound is progressing, whether infection is developing, and whether adjustments to care are needed. Recognizing the right time and reason to change a dressing is essential to maintaining both wound health and patient comfort.
1. Loose or Poor Adhesion
If the dressing is no longer properly adhered to the skin, it can no longer provide an effective barrier against bacteria and dirt. This can lead to contamination and increase the risk of infection. If you notice the dressing lifting or moving around, it is time to change it.
2. Exudate Saturation
When a dressing becomes saturated with exudate , it can no longer absorb additional exudate, and the wound may become exposed to moisture, which can harm the surrounding skin. In this case, the dressing should be replaced to prevent maceration and encourage optimal healing conditions.
3. Signs of Infection
If you notice any signs of infection, such as redness, swelling, odor, or increased pain, it is critical to change the dressing immediately. Infection can significantly delay healing and even cause serious complications, so timely intervention is necessary.
4. Clinical Reassessment
Healthcare providers may need to reassess the wound to determine if the healing process is progressing as expected. In such cases, the dressing should be removed temporarily for a thorough evaluation.
With advanced wound dressings, the number of dressing changes can often be reduced. For example, the R&L Visual Waterproof Dressing combines an absorbent honeycomb foam layer with a transparent polyurethane film. This design controls exudate effectively while allowing the wound to be visually monitored without removal. As a result, patients benefit from fewer unnecessary dressing changes, less pain and disruption, and a more stable healing environment. For clinicians, this means better wound management and improved efficiency in care delivery.
-
Reduced infection risk: providing a secure barrier against bacteria and viruses.
-
Longer wear time: minimizing the frequency of dressing changes, which reduces disruption to the wound.
-
Patient-centered design: flexibility, breathability, and low allergenic potential for improved quality of life.
At R&L Medical, our mission is to lead in this new generation of wound care, offering products that deliver these benefits in real clinical practice.
Post Surgical Wound Dressing
Surgical wounds present unique challenges. They must remain protected from bacteria while the incision heals, but they also need to allow physicians to observe the site for signs of infection or dehiscence (wound reopening). Post-surgical dressings should:
-
Provide waterproof and bacteria-resistant protection.
-
Offer gentle adhesion to avoid damaging delicate skin during removal.
-
Stay securely in place over moving body parts.
-
Reduce the frequency of dressing changes to minimize infection risk and improve comfort.
Our dressings play an important role in postoperative recovery by protecting the incision and supporting faster, cleaner healing. They are especially suitable for surgical sites with low to moderate exudate, helping maintain a moist healing environment while preventing contamination. At R&L Medical, we design dressings that balance secure adhesion with comfort, ensuring patients can recover confidently at home.
Advantages of visual waterproof dressings for this type of disease
-
Flexible: conforming to knee movement without losing adhesion.
-
Absorbent: capable of managing moderate exudate during the early recovery period.
-
Waterproof: enabling patients to maintain hygiene and shower without compromising protection.
-
Durable: remaining intact despite bending and stretching.

When and Why Change Dressing on Wound Changing a wound dressing is more than just a scheduled task; it is also an opportunity to assess the healing process and identify potential complications early. Each dressing change gives clinicians and patients the chance to evaluate how well the wound is progressing, whether infection is developing, and whether adjustments to care are needed. Recognizing the right time and reason to change a dressing is essential to maintaining both wound health and patient comfort.
1. Loose or Poor Adhesion
If the dressing is no longer properly adhered to the skin, it can no longer provide an effective barrier against bacteria and dirt. This can lead to contamination and increase the risk of infection. If you notice the dressing lifting or moving around, it is time to change it.
2. Exudate Saturation
When a dressing becomes saturated with exudate , it can no longer absorb additional exudate, and the wound may become exposed to moisture, which can harm the surrounding skin. In this case, the dressing should be replaced to prevent maceration and encourage optimal healing conditions.
3. Signs of Infection
If you notice any signs of infection, such as redness, swelling, odor, or increased pain, it is critical to change the dressing immediately. Infection can significantly delay healing and even cause serious complications, so timely intervention is necessary.
4. Clinical Reassessment
Healthcare providers may need to reassess the wound to determine if the healing process is progressing as expected. In such cases, the dressing should be removed temporarily for a thorough evaluation.
With advanced wound dressings, the number of dressing changes can often be reduced. For example, the R&L Visual Waterproof Dressing combines an absorbent honeycomb foam layer with a transparent polyurethane film. This design controls exudate effectively while allowing the wound to be visually monitored without removal. As a result, patients benefit from fewer unnecessary dressing changes, less pain and disruption, and a more stable healing environment. For clinicians, this means better wound management and improved efficiency in care delivery.
How Often to Change Dressing on Wound
One of the most common concerns for patients and caregivers in wound care is: how often should a dressing be changed? The answer is not one-size-fits-all. The frequency depends on the nature of the wound, the dressing material, and the overall healing progress. Changing too often may disturb the wound bed and slow healing, while changing too infrequently can increase the risk of infection. Striking the right balance is key to effective wound management.
-
Wound type: Acute wounds such as minor cuts or surgical incisions usually need less frequent changes, while chronic wounds like pressure ulcers or diabetic ulcers require closer monitoring and more frequent intervention.
-
Exudate levels: Heavily draining wounds demand regular dressing changes to manage fluid, while low-exudate wounds can be covered for longer periods.
-
Type of dressing: Traditional gauze absorbs poorly and often requires daily changes. In contrast, advanced dressings like foams, hydrocolloids, and transparent films are designed to extend wear time, sometimes lasting several days.
-
Signs of contamination: Any dressing showing leakage, odor, or visible soiling must be changed immediately to prevent bacterial growth and infection.
Traditional gauze dressings may need to be replaced once or even multiple times per day, which can be uncomfortable for patients and labor-intensive for caregivers. Advanced wound dressings, on the other hand, provide longer protection and greater comfort. By allowing extended wear while maintaining a moist, protective environment, they not only reduce the burden of frequent changes but also support uninterrupted healing. For patients and clinicians alike, this represents a major step forward in modern wound care.
Change Dressing on Wound
Proper dressing change is vital for wound healing. Following a structured routine helps reduce infection risk and ensures the dressing performs as intended. Here is a simple step-by-step guide:
Step 1: Wash Hands Thoroughly
Always start by washing your hands with soap and water for at least 20 seconds. If available, put on disposable medical gloves. This minimizes the chance of transferring bacteria to the wound.
Step 2: Gently Remove the Old Dressing
Carefully peel away the dressing, supporting the skin to avoid pulling. Take your time to prevent pain or damage to fragile new tissue. Advanced non-stick dressings make this step easier by minimizing trauma.
Step 3: Cleanse the Wound
Use sterile saline or a wound cleanser recommended by your healthcare provider. This helps remove debris and bacteria without irritating the wound. Avoid using harsh antiseptics unless specifically prescribed.
Step 4: Dry the Surrounding Skin
Pat the skin around the wound gently with sterile gauze until completely dry. This ensures better adhesion for the new dressing and helps prevent edges from lifting prematurely.
Step 5: Apply the New Dressing
Place the fresh dressing carefully over the wound, ensuring full coverage. Press the edges gently to seal, creating a barrier against water, dirt, and bacteria.
Pro Tip: Best practices also include minimizing unnecessary dressing changes. Advanced products, such as the R&L Visual Waterproof Dressing, enable clinicians and patients to check wound status without removal, reducing the risk of infection and preserving the healing environment.
Best Dressing for Open Wound
Open wounds, including lacerations, abrasions, and chronic ulcers, present unique challenges for both patients and clinicians. Unlike closed surgical incisions, open wounds are more vulnerable to infection, excessive fluid loss, and delayed healing. Choosing the best wound dressing depends on the wound’s depth, size, exudate level, and risk of contamination. Advanced dressings are particularly effective because they not only protect the wound surface but also create an environment that accelerates tissue regeneration while reducing discomfort.
Foam Dressings
Foam dressings are ideal for wounds with moderate to heavy exudate. Their highly absorbent structure manages wound fluid efficiently, preventing skin maceration around the wound edges. They also provide cushioning, which reduces pain and protects against external pressure or friction. Foam dressings are commonly used for pressure ulcers, traumatic injuries, and post-surgical wounds that produce significant drainage.
Alginate Dressings
Alginate dressings, made from natural seaweed fibers, are another excellent choice for heavily draining wounds. When in contact with exudate, alginates form a soft gel that conforms to the wound bed, maintaining a moist environment while trapping excess fluid. They are especially effective for deep cavity wounds or infected ulcers. In addition to absorption, alginate dressings promote hemostasis, making them useful for bleeding wounds.
Hydrocolloid Dressings
Hydrocolloid dressings are best suited for wounds with low to moderate exudate. These dressings contain hydrophilic particles that interact with wound fluid to create a moist healing environment, which supports granulation and epithelialization. Hydrocolloids are particularly beneficial for superficial abrasions, minor burns, and pressure sores. They also help minimize pain during dressing changes because they do not adhere strongly to the wound bed.
Transparent Film Dressings
Transparent film dressings are thin, flexible sheets that provide a waterproof yet breathable barrier. They are most appropriate for superficial open wounds such as abrasions or surgical sites with minimal exudate. Their transparency allows for real-time visual monitoring without removing the dressing, reducing unnecessary disruption. Patients can continue daily activities, including showering, while maintaining wound protection.
Transparent Film Dressing Is Used for Which Type of Wound?
Transparent film dressings are thin polyurethane sheets coated with a medical-grade adhesive. Their unique properties make them particularly useful for:
-
Post-surgical incisions: providing waterproof protection while allowing visual inspection.
-
Superficial abrasions: covering shallow wounds that require protection but minimal exudate management.
-
IV line sites: securing catheter entry points while preventing contamination.
-
Joints and curved surfaces: adapting to body movement without peeling.
The main advantage of transparent film dressings is Visual. Clinicians and patients can monitor healing without removing the dressing, minimizing unnecessary disturbances to the wound. In addition, their waterproof nature allows patients to shower with confidence, improving quality of life during recovery.
There is no single “best dressing” for all open wounds. The choice depends on wound size, depth, exudate level, and infection risk. What advanced dressings share in common, however, is their ability to balance moisture, protect against infection, and support faster recovery compared to traditional options.
How to Reduce Dressing Change Frequency
At R&L Medical, one of our core innovations is reducing the burden of frequent dressing changes. Traditional wound care often involves changing the dressing multiple times a day, which can be painful, disruptive, and time-consuming. This frequent removal and reapplication can also hinder healing, increase the risk of infection, and cause unnecessary discomfort. Our Visual Waterproof Dressing is designed to address these challenges by extending wear time, providing a secure and protective barrier, and minimizing the need for constant dressing changes.
Our Visual Waterproof Dressing is engineered with three key layers:
Top Layer: Transparent Polyurethane Film
The top layer is a transparent polyurethane film that provides waterproof and bacteria-resistant protection. This layer ensures that the wound is shielded from external contaminants, including water, dirt, and pathogens. Its transparent nature also allows for visual monitoring of the wound without the need to remove the dressing, reducing disruption and minimizing the risk of infection.
Middle Layer: Honeycomb Foam
The middle layer of the dressing is made of honeycomb foam, which absorbs wound exudate efficiently. This foam structure helps manage moisture levels, preventing both excessive moisture and drying out of the wound bed. It also provides cushioning to protect the wound from external pressures or impacts, contributing to both faster healing and greater comfort for the patient.It also provides a moist treatment environment to help wounds heal quickly.
Bottom Layer: Non-Adhesive Contact Layer
The bottom layer is a non-adhesive contact layer, designed to prevent trauma during dressing removal. Unlike traditional dressings that can stick to the wound, causing pain or tissue damage when removed, this layer ensures that the dressing does not adhere to the wound bed, making removal painless and minimizing the risk of further injury to healing tissue.
The result of this multi-layer structure is several key advantages:
-
Visual monitoring: With the transparent top layer, healthcare providers and patients can check the wound without needing to remove the dressing, allowing for better wound tracking and less disruption.
-
Waterproof protection: The waterproof film ensures patients can shower, bathe, or swim without worrying about the dressing becoming wet or ineffective.
-
High absorbency and breathability: The honeycomb foam maintains a moist wound environment, essential for faster healing, while still being breathable to prevent maceration and irritation.
By minimizing the need for frequent dressing changes, R&L Visual Waterproof Dressing reduces the risk of infection, minimizes disruption to the wound, and greatly enhances patient quality of life. This extended wear time means fewer dressing changes, less pain, and a more comfortable recovery. Our innovative design allows the body to heal more naturally, efficiently, and with greater confidence.
Conclusion
Advanced wound dressings are transforming the way we approach wound care. By combining moisture management, infection prevention, and patient-centered design, they provide superior outcomes compared to traditional dressings. From transparent films for surgical sites to foams and alginates for exudative wounds, these innovations serve a wide range of clinical needs.
At R&L Medical, we are proud to contribute to this transformation with our Visual Waterproof Dressing. By enabling real-time visibility, waterproof protection, high absorbency, and reduced dressing-change frequency, we offer patients and healthcare providers a truly advanced solution. Whether for post-surgical care, diabetic ulcer management, or orthopedic recovery, our products are designed to set a new benchmark in wound healing.
For patients, caregivers, and clinicians alike, the future of wound care is clear: advanced dressings are not just an option—they are the new standard.
At the same time, our dressings have been approved by the Malaysia MDA, Singapore HSA, and Vietnam MOH. These certifications confirm their quality, safety, and clinical reliability, and provide a strong foundation for expanding the clinical use of our advanced wound care products in overseas markets.
